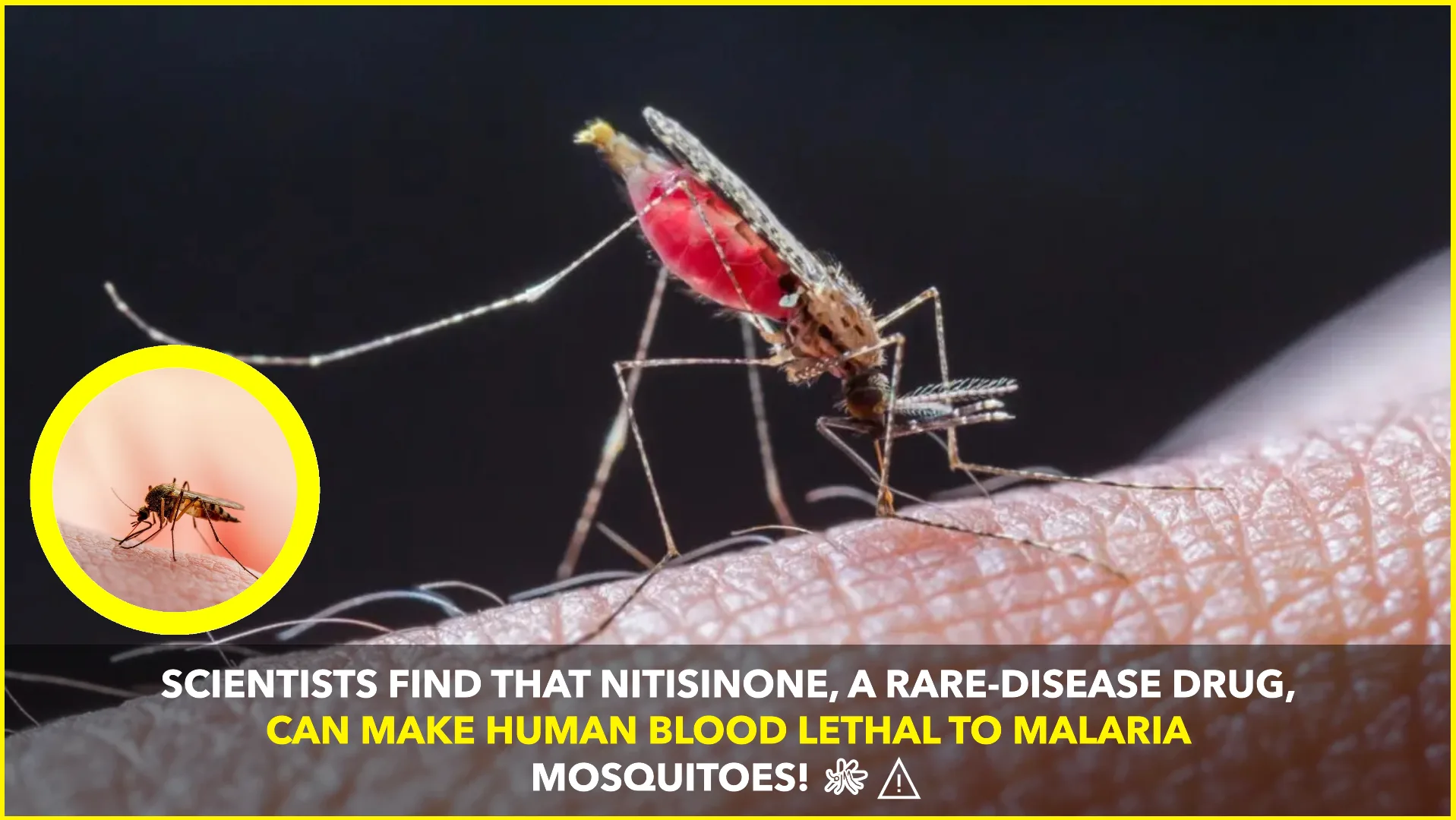
In a groundbreaking development in the fight against malaria, scientists have discovered that nitisinone—a drug traditionally used to treat rare genetic disorders—can render human blood lethal to malaria-carrying mosquitoes. This finding opens new avenues for malaria control by potentially reducing mosquito populations and interrupting disease transmission.
Nitisinone, an FDA-approved medication, has been primarily employed to manage conditions like hereditary tyrosinemia type I and alkaptonuria. Its mechanism involves inhibiting the enzyme 4-hydroxyphenylpyruvate dioxygenase (HPPD), which plays a crucial role in tyrosine metabolism. Recent studies have illuminated its unexpected efficacy against blood-feeding insects.
Research led by Dr. Álvaro Acosta-Serrano at the Liverpool School of Tropical Medicine demonstrated that nitisinone is lethal to tsetse flies, vectors of African trypanosomiasis. The drug disrupts the flies’ ability to degrade tyrosine obtained from blood meals, leading to toxic accumulation and subsequent death. Importantly, this effect was specific to blood-feeding insects, as non-hematophagous species like bumblebees remained unaffected when exposed to the drug.
Building upon these findings, a collaborative study involving researchers such as Anna Trett and Lee Haines explored nitisinone’s impact on malaria-transmitting mosquitoes. The study revealed that when mosquitoes fed on human blood containing nitisinone, they experienced high mortality rates, irrespective of their age or resistance to existing insecticides. Furthermore, individuals with alkaptonuria, who are administered low daily doses of nitisinone (2 mg/day), were found to have blood that is toxic to mosquitoes. This suggests that nitisinone could serve as a novel tool in malaria control strategies. Figshare+1DDN Magazine+1
The potential applications of nitisinone in vector control are vast. Administering the drug to at-risk human or animal populations could transform them into systemic agents against mosquitoes, thereby reducing the prevalence of malaria and other vector-borne diseases. This approach offers an innovative complement to existing control measures, especially in regions where insecticide resistance poses a significant challenge.
The specificity of nitisinone’s action is particularly noteworthy. Unlike broad-spectrum insecticides that can harm beneficial insect populations, nitisinone targets the unique metabolic pathways of blood-feeding insects. This selectivity minimizes ecological disruption and underscores the drug’s potential as an environmentally friendly alternative in vector management.
While these findings are promising, further research is necessary to fully understand the implications of nitisinone use in humans and its long-term effects on mosquito populations. Field studies are essential to assess the practicality of implementing nitisinone-based interventions in diverse ecological settings. Additionally, evaluating the potential for mosquitoes to develop resistance to nitisinone will be crucial in ensuring the sustained efficacy of this approach.
The repurposing of nitisinone exemplifies the innovative strategies being explored to combat malaria—a disease that continues to exert a heavy toll on global health. By leveraging existing medications in novel ways, researchers are expanding the arsenal of tools available to reduce the burden of vector-borne diseases. As studies progress, nitisinone could become a pivotal component in integrated malaria control programs, offering hope for millions affected by this devastating illness.